This Policy Brief examines prescription drug takeback programs in the context of substance abuse prevention. Across America, drug takeback programs have become increasingly popular as policymakers struggle to provide individuals with a secure and convenient way to dispose of unused medications. To learn more about takeback programs, Carnevale Associates, LLC surveyed a number of programs to better understand their design, costs, and efficacy to support national efforts to reduce the size and scope of the prescription drug epidemic. Our analysis found that these programs vary substantially in cost and approach. In addition, we found no evidence that takeback programs affect prescription drug abuse. We conclude that additional research is needed before incorporating takebacks into any substance abuse prevention plan.
Download the PDF: Prescription Drug Takeback Programs & Substance Abuse Policy
Prescription Drug Takeback Programs & Substance Abuse Policy
Introduction
Now recognized as an epidemic and identified in President Obama’s 2011 National Drug Control Strategy as “America’s fastest-growing drug problem,” non-medical use of prescription drugs outpaces all other illegal drug use except marijuana (1). To combat the growing non-medical use of prescription drugs, the Office of National Drug Control Policy (ONDCP) released a Prescription Drug Abuse Prevention Plan, outlining a four-pronged effort of (1) education, (2) monitoring, (3) proper medication disposal, and (4) enforcement. Across America, drug takeback programs have become increasingly popular as policymakers struggle to provide individuals with a secure and convenient way to dispose of unused medications. Though takeback programs differ considerably, all takebacks accept some types of unused medication. To learn more about takeback programs, Carnevale Associates, LLC surveyed a number of programs to better understand their design, costs, and efficacy to support national efforts to reduce the size and scope of the prescription drug epidemic. Our analysis found that these programs vary substantially in cost and approach. In addition, we found no evidence that takeback programs affect prescription drug abuse. We conclude that additional research is needed before incorporating takebacks into any substance abuse prevention plan (2).
Prescription Drugs: The New Epidemic
Non-medical use of prescription drugs is now at record levels and shows no signs of slowing. Growing numbers of first-time users (initiates) point to a continuing trend of increased use. According to the ubstance Abuse and Mental Health Administration’s (SAMHSA) 2010 National Survey on Drug Use and Health (NSDUH), 7 million Americans used prescription drugs non-medically in the past month (current use). In addition, 16 million Americans used a prescription drug non-medically at least once in 2010, up 8 percent since 2002 (14.8 million). In fact, every year since 2002, 2.4 to 2.8 million Americans have used prescription drugs non-medically for the first time, with prescription pain relievers now attracting new users at a rate outpacing all drugs but marijuana.
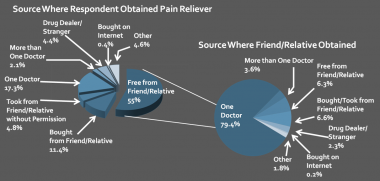
Importantly, the NSDUH shows that over half of the individuals who used prescription drugs non-medically in the past year obtained their drugs free from a friend or relative. Examining detailed data on prescription pain relievers (which constitute the majority of non-medical use), 55 percent of users obtained drugs free from a friend/relative, 11.4 percent bought them from a friend/relative, and 4.8 percent took them from a friend/relative without asking (See Figure 1). In total, 71 percent cited friends/relatives as the immediate source of their drug supply; however, nearly 94 percent of those individuals reported that their friends/relatives were willing partners in the diversion.
Takeback Programs: Overview
Because most non-medical prescription drug users obtain their drugs from friends/relatives, substance abuse prevention efforts have increasingly targeted the family medicine cabinet—attempting to cut off supply by offering a safe and secure method for drug disposal. In light of their growing popularity, Carnevale Associates conducted a survey of takeback programs, examining data from 148 programs spanning 21 states and several countries. Our analysis found that takebacks vary considerably. While all takebacks accept some types of unused medication, takeback programs often have different goals, structure, and scope. Based on our findings, programs vary across five interrelated elements: (1) frequency, (2) collection mechanism, (3) drugs accepted, (4) collecting entity, and (5) geographic scope.
- Frequency: Takebacks can be classified as either “event-based” or “ongoing.” Event-based programs offer sporadic pre-scheduled collections on fixed dates. The most notable example of these is the Drug Enforcement Administration (DEA) Takeback Days. In contrast, ongoing programs offer some form continuous medication collection, featuring either fixed drop-off locations (e.g. pharmacies or police stations) or an option to mailback unused drugs.
- Collection Mechanism: Takebacks can be classified as either “bin-based,” “mailback,” or “person-facilitated.” Bin-based collections utilize specially designed locking containers into which individuals directly deposit unused drugs, mailback collections utilize USPS-based return envelopes, and “person-facilitated” collections direct participants to transfer drugs directly to designated takeback personnel (predominantly at event-based collections).
- Drugs Accepted: Only some takebacks accept controlled medications—the drugs targeted by substance abuse prevention programs. Under current law, only law enforcement may accept controlled substances. As a result, only takebacks located at law enforcement facilities or working with law enforcement entities may accept controlled drugs (3). Nearly all takebacks accept non-prescription medication (e.g. Tylenol or vitamins) in addition to uncontrolled prescription medication (e.g. antibiotics).
Assessing Takebacks: Little is Known
Despite their proliferation, little data is available on the impact and effectiveness of takeback programs. In fact, no research has been conducted to investigate takebacks’ effect on prescription drug abuse. Though takebacks necessarily reduce the available supply of prescription drugs, voluntary programs are unlikely to draw participation from individuals inclined towards diversion or non-medical use. While 66 percent of non-medical users report that friends/relatives were willing participants in diversion, only 4.8 percent obtained drugs from friends/relatives without their permission. Consequently, takebacks may reduce supply without measurably affecting abuse. In addition, Figure 1 shows that most individuals diverting unused drugs originally obtain those drugs from a single doctor, highlighting doctors as the ultimate source of the drug surplus rather than the family medicine cabinet. These data suggest that policymakers may have more success focusing on overprescribing behavior within the medical community rather than on surplus drugs already in individuals’ homes. In fact, a study by Simeone and Associates, Inc. found that states with prescription drug monitoring programs (PDMPs) that proactively monitor prescribing behavior have a lower likelihood of opioid abuse (4).
Carnevale Associates’ analysis found that only 11 percent of the domestic takeback programs surveyed collected data on both costs and medications received. In addition, because of their structure, many programs do not collect controlled substances at all. With few exceptions, those programs that do collect controlled drugs make no effort to determine what percentage of their collections are controlled. To determine takebacks’ effectiveness as substance abuse prevention programs, policymakers must know both how much controlled medication they receive and how much the collections cost. Though some programs (notably, Maine’s Safe Disposal for ME mailback program) do collect these data, they are not representative of other takebacks and therefore cannot inform a national assessment.
Limited data from our analysis suggest that takebacks’ efficiency varies by program characteristics. Our data show that mailback programs cost $62 per pound of collected medication, event-based programs cost $42 per lb., and ongoing bin-based collections cost $7 per lb. Though not statistically significant because of paucity of data, these findings provide a guiding point for future research and real-time policy decisions, indicating that some takeback structures may be considerably more cost-efficient than others.
Recommendations: Further Research
To address these data gaps and help policymakers target limited prevention resources, Carnevale Associates recommends:
- Conducting takeback pilots to determine which medications are collected, assess takebacks’ true costs, and link elements of programmatic structure with costs and collections
- Researching the relationship between prescription drug abuse and takeback programs
- Updating the research on PDMPs’ contribution to reducing prescription drug abuse and comparing PDMPs to takeback programs
- Focusing takeback resources on the most cost efficient takebacks until additional data are available
While epidemics often require swift action in advance of research, without these data, takeback programs will remain untested policy. Though potentially useful, such programs may also draw limited prevention resources away from more effective programs, policies, and practices. Similarly, research may link takebacks’ effectiveness to certain programmatic features, which may help conserve limited prevention dollars.
Conclusion
The prescription drug epidemic is the new frontier of substance abuse policy. Safe and secure disposal of unused medication must be an important component of substance abuse prevention. However, given the dearth of information on takeback programs, more research is needed before heavily investing in takebacks as a key component of substance abuse prevention strategy. Until research can properly assess the effectiveness and cost-effectiveness of takebacks, scare prevention resources should fund proven policies, programs, and practices, including PDMPs and programs to modify providers’ prescribing behavior. Policymakers must seek new solutions to emerging drug problems; however, in these austere times, they must also be careful to allocate scarce prevention dollars to prevention programs that will do the most good.
Notes:
- Drug use statistics exclude underage use of alcohol and cigarettes.
- This brief does not assess takebacks' value as environmental programs.
- The U.S. DOJ is currently writing regulations to implement the Safe and Secure Drug Disposal Act of 2010, which may alter this law.
- Simeone, R. & Holland, L. An evaluation of prescription drug monitoring programs. NCJRS (NCJ217269), US DOJ, Washington DC, 2006.